What are the 5 Major Symptoms of Narcolepsy
Narcolepsy is a permanent neurological disease that disrupts sleep-wake homeostasis, consequently defining deep daydreaming and, in some instances, sleep collapse. The following additional symptoms are primarily observed: excessive daytime sleepiness, cataplexy (muscle weakness triggered by emotional reactions), sleep paralysis, hallucinations during sleep onset or awakening, and disruption of nocturnal sleep continuity. The severity of symptoms varies significantly, and early identification cannot be overlooked in management. Accurate diagnosis and therapeutic intervention have been identified as the core steps to achieving positive outcomes and overall improvement in quality of life by the NHS and other medical organizations. When a diagnosis is suspected, consulting professionals is highly advisable.
Section 1: Understanding Narcolepsy
What Is Narcolepsy?
Narcolepsy is a sleep disorder of a chronic nature with symptoms of excess daytime sleepiness and deviant sleep-wake cycle. People with this condition can still feel sleepy throughout the day, even after getting enough sleep at night. There are two main subtypes; type 1 is characterized by a sudden, involuntary loss of muscular strength (cataplexy), and type 2 lacks that manifestation. Some of them can be defined as mild cases of narcolepsy when the symptoms are diminished but still interfere with normal functioning. By proper diagnosis and management, the quality of life among individuals who go through narcolepsy can be improved.
How Common Is Narcolepsy?
Narcolepsy is also a proportionate but causal sleep illness that affects one person in 2,000. The state often goes unnoticed, with alarmingly small symptoms, like excessive daytime sleepiness, frequently passed off as fatigue or insomnia. Closer communication with the population and thorough medical assessment would be essential in providing accurate diagnoses and effective follow-up with appropriate treatment measures.
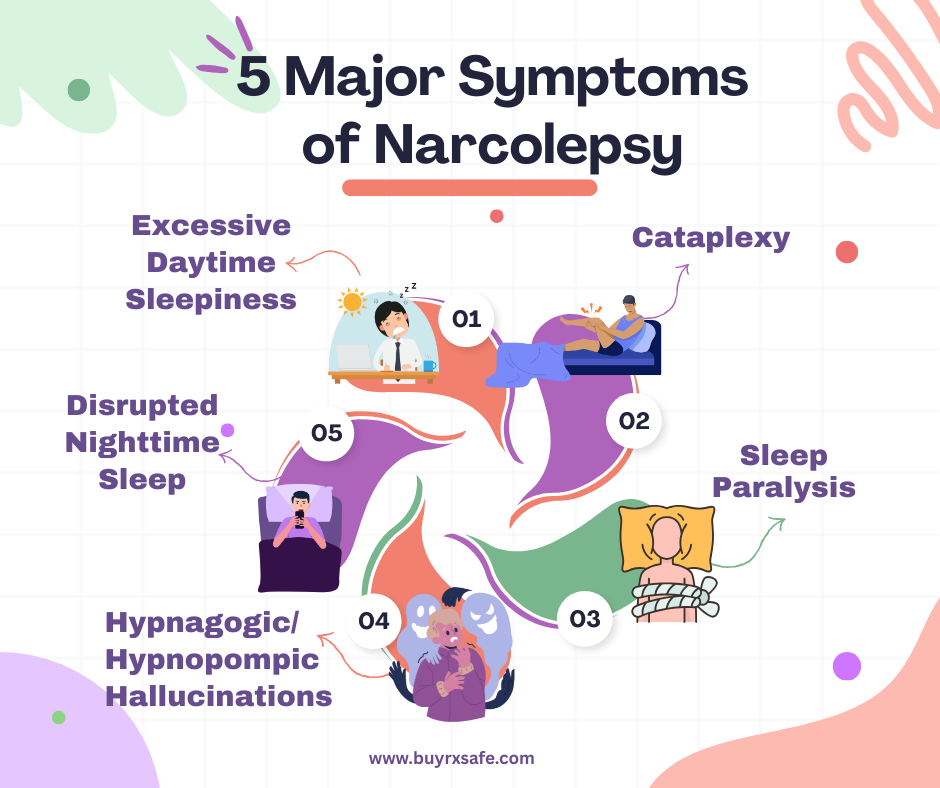
Section 2: The 5 Major Symptoms of Narcolepsy
Narcolepsy has five significant symptoms: excessive daytime sleepiness, sudden loss of muscular tone (cataplexy), sleep paralysis, hallucinated hypnagogic images during the process of falling asleep or waking up, and not getting enough quality sleep during the night. Such clinical characteristics significantly disrupt normal functioning in daily life and, therefore, require strict medical analysis and treatment.
1. Excessive Daytime Sleepiness (EDS)
Constant Sleepiness: Individuals with narcolepsy often experience a persistent urge to sleep during the day despite having slept for an entire night. This feeling is quite different from normal tiredness; it is abrupt and, to a large extent, beyond control.
Inhibition of Everyday Function: Excessive daytime sleepiness (EDS) can impair cognition and productivity, interfere with an individual's safety, and subsequently make routine daily activities, including work, driving, and everyday social functioning, extremely challenging. A considerable number of victims find it hard to be vigilant during a meeting or on the road.
Attacks Without Warning: Sleep attacks may occur at any time, often with no prior warning, forcing the person to take frequent naps to remain productive.
2. Cataplexy (Sudden Muscle Weakness)
Triggered by emotions: Cataplexy is an emotionally triggered condition that causes sudden muscle weakness or collapse, typically triggered by strong emotional reactions such as laughing, becoming angry, or experiencing extreme excitement. It is primarily associated with Narcolepsy type 1, although it may not be exhibited in Narcolepsy type 2 (NHS).
Varies in severity: The acuteness of manifestation is great; severe attacks lead to complete somatic breakdown, while temporarily weaker forms exhibit slight symptoms, such as drooping eyelids or slurred speech. Such a diagnosis is crucial for distinguishing this phenomenon and related disorders.
Linked to sleep regulation: It has been evidenced that loss of muscular control is due to rapid-eye-movement (REM) sleep regulation impairment, and cataplexy has emerged as one of the diagnostic features of narcolepsy. The sooner it is recognized, the more it can be managed and the higher the general quality of life.
3. Sleep Paralysis
Sleep paralysis, a temporary inability to move the skeletal and muscular systems, is often associated with the development of narcolepsy and may be experienced upon waking up or falling asleep. A victim can be completely still and unable to communicate within a small time frame, commonly a few seconds or minutes, which can be highly anxiety-inducing. At the same time, there is a tendency to report hallucinatory phenomena, a sense of the presence of something intrusive in the room, or the apparent presence of shadowy forms.
Slightly morbid though it is, sleep paralysis remains non-pathological in physiological terms and usually clears up on its own. Self-management techniques, such as practicing conscious, rhythmic breathing, help facilitate recovery. When the attacks are repeated, it is beneficial to address a specialist in the field of sleep to get a thorough assessment and optimization of therapy. The occurrence of sleep paralysis contributes to the importance of proper diagnosis and effective treatment of the issue of managing narcolepsy.
4. Hypnagogic/Hypnopompic Hallucinations
Narcolepsy may generate thrilling dreamlike hallucinations that occur in gentle bedevilment (hypnagogic) or during dawning (hypnopompic). These hallucinations are most likely to sound, look, or even feel incredibly realistic and may be downright disturbing. Often, people mistake such phenomena as paranoia symptoms and do not realise that the violation of the healthy sleep-wake mode causes these.
The origin of such hallucinations can be traced to the premature entry of the brain into a state of rapid-eye movement (REM) sleep, during which dreaming occurs without the person's awareness. Since the content of dreams and the conscious state become intertwined, the experience may be confusing. Understanding that these episodes occur as a manifestation of narcolepsy makes it easy to intervene and make a diagnosis. Visiting a sleep specialist can help clarify the condition and provide a set of strategies for reducing its occurrences and mitigating its impact.
5. Disrupted Nighttime Sleep
Narcolepsy disrupts nighttime sleep through the generation of frequent nocturnal awakenings, accompanied by daytime drowsiness and excessive daytime sleepiness. Unlike insomnia, where a person cannot sleep or sleep properly due to increased alertness, fragmented sleep, in the case of narcolepsy, is related to disturbed patterns of the sleep-wake cycle. The victim wakes up violently and is easily able to go back to sleep, but in the case of insomnia patients, they go through long periods of not sleeping.
In addition, one of the significant symptoms of narcolepsy is disoriented sleep caused by the intrusion of REM sleep, which is mainly associated with powerful dreams and nightmares. It is not very common to encounter these REM disturbances in insomnia, and instead, it is directly related to stress or anxiety. The two diseases lead to fatigue, although in narcolepsy, sleep disturbances are part of a neurologic disorder as opposed to simply not being in a position to sleep well.
Section 3: Mild Narcolepsy – Can You Have a Mild Form?
Mind you, a mild form of narcolepsy is possible. This makes it less disruptive as even patients with mild symptomatology can complain of a weak level of somnolence during the day, minor disturbances of concentration, and lapses of attention, all of which are free of significant sleep attacks and cataplexy.
Yes, there is such a mild form of narcolepsy, but the attenuation of its symptoms can identify it. Mild cases of narcolepsy are marked by frequent sleep attacks, as opposed to the constant feeling of fatigue that is present in more severe cases. Muscle limpness, as QS, e.g., drooping of eyelids, etc., is another and more modest manifestation of the strength loss than the total breakdown of less advanced forms. Such subtle statements help numerous patients spend their days somewhat efficiently yet still face significant struggles.
Since the symptoms of narcolepsy are mild, it can be pretty challenging to give an accurate diagnosis. Doctors may dismiss these symptoms as unimportant or misunderstand them as mere exhaustion or mental stress. When suspicion develops, a sleep expert may, however, resort to tests such as the polysomnogram or multiple sleep latency tests to confirm or dispel the suspicion. Accurate diagnosis is essential for effectively controlling symptoms.
Section 4: What Narcolepsy Looks Like in Daily Life
Real-life examples of how symptoms manifest:
The disease causes a significant disturbance in routine life since instant, irresistible sleep attacks and provisional muscle weakness occur. Such individuals can even fall asleep in the middle of a discussion while eating or while driving, therefore making several other everyday activities problematic. Cataplexy, a sudden loss of muscular control, can occur as a drop of the head, slurred speech, or total collapse, often provoked by strong emotional stimuli, such as laughter or surprise.
In learning institutions and the workplace, chronic daytime sleepiness leads to loss of concentration, memory impairments, and reduced productivity. Most patients struggle to stay awake during meetings or classes and often rely on brief naps to remain alert. Simple-looking activities can also be tedious, and embarrassment factors can hamper social interactions during symptomatic episodes. Narcoleptics, therefore, have to adjust their lives all the time to have some semblance of an everyday life.
Differences between mild and severe cases.
Narcolepsy provides a gross impairment of everyday functioning, including endemic daytime somnolence, in addition to periodic sleep attacks as well as disjointed sleep during the night. On a milder scale, an individual may experience a state of temporary drowsiness or short-term insomnia. In its most extreme forms, the condition may manifest itself through the signs of cataplexy (loss of instant muscle tone), sleeping paralysis, and hallucinations. Affecting functions such as driving or long-term employment, these symptoms interfere with activity, and sleepiness is often inevitable.
Section 5: Diagnosis and Treatment
Doctors identify disease through a series of rigorous tests and complementary tests, as well as the patient's medical history. Such treatment plan interventions can include pharmacotherapy, psychotherapy, and surgery, all of which can be highly tailored to the individual to achieve the most excellent recovery.
How Is Narcolepsy Diagnosed?
During the clinical evaluation of narcolepsy, doctors typically use two types of sleep testing: polysomnography (PSG) and the Multiple Sleep Latency Test (MSLT). The former measures the structure of nighttime sleep, whereas the latter measures day somnolence by measuring the time it takes to fall asleep when conditions are quiet.
The National Health Service recommends that individuals who report extreme daytime sleepiness or sudden muscle weakness, often accompanied by conditions such as cataplexy, should be evaluated by a specialized sleep expert. Narcolepsy types 1 and 2 are distinguished through a diagnosis conducted according to the ideal systematic evaluation of clinical evidence and test results. Early diagnosis leads to timely treatment, and this can include treatment with stimulants, antidepressants, or long-standing lifestyle alterations.
Treatment Options
Both lifestyle interventions and pharmacotherapy are usually used in managing Narcolepsy. Sodium oxybate improves nocturnal sleeping disorders and their symptoms; stimulants and antidepressants help decrease sleepiness and cataplexy experienced during the day. Regular sleep and strict sleep hygiene help counter fatigue further.
Emotional support can be obtained through supportive networks and psychotherapy, enabling patients to manage better the challenges associated with their condition. Treatment planning, combined with the early manifestation of the disease, significantly improves the quality of life. Communication with a sleep expert remains crucial in establishing an even more effective treatment regimen.
Conclusion
There are five main manifestations of narcolepsy: excessive daytime sleepiness (EDS), sudden loss of body control (cataplexy), nighttime sleep disturbance, sleep paralysis, and vivid hallucinations during the process of sleep-wake transitions. The offenses on this scale can easily affect everyday functioning and can not be ignored. Individuals experiencing these symptoms are advised to consult a healthcare practitioner for a proper diagnosis and treatment. Further instructions can be found at the NHS site or through contact with narcolepsy support groups. Prevention with early diagnosis will result in a significant improvement in general living standards.